+86 178 5514 5298
+86 178 5514 5298
Leave Your Message
-
 CONTACT NUMBER
CONTACT NUMBER -
 CONTACT NUMBER
CONTACT NUMBER -
 CONTACT NUMBER
CONTACT NUMBER



The collection of blood samples is crucial in clinical testing. The right blood sample collection tubes ensure accurate results. According to a report by Global Market Insights, the global market for blood collection tubes is projected to reach USD 6.8 billion by 2026. This growing demand highlights the importance of understanding tube types and their uses.
Dr. Emily Chen, a leading expert in clinical diagnostics, states, “Selecting the appropriate blood collection tubes directly influences test outcomes.” Her insight underscores a key issue. Many professionals still struggle with tube selection and handling. Mismatches can lead to erroneous results and patient misdiagnosis.
As the industry evolves, more education is needed. Proper training on blood sample collection tubes can reduce errors and enhance accuracy. Continuous improvement and learning are essential. We must reflect on existing protocols. Are they the best? There's always room for enhancement in practice.

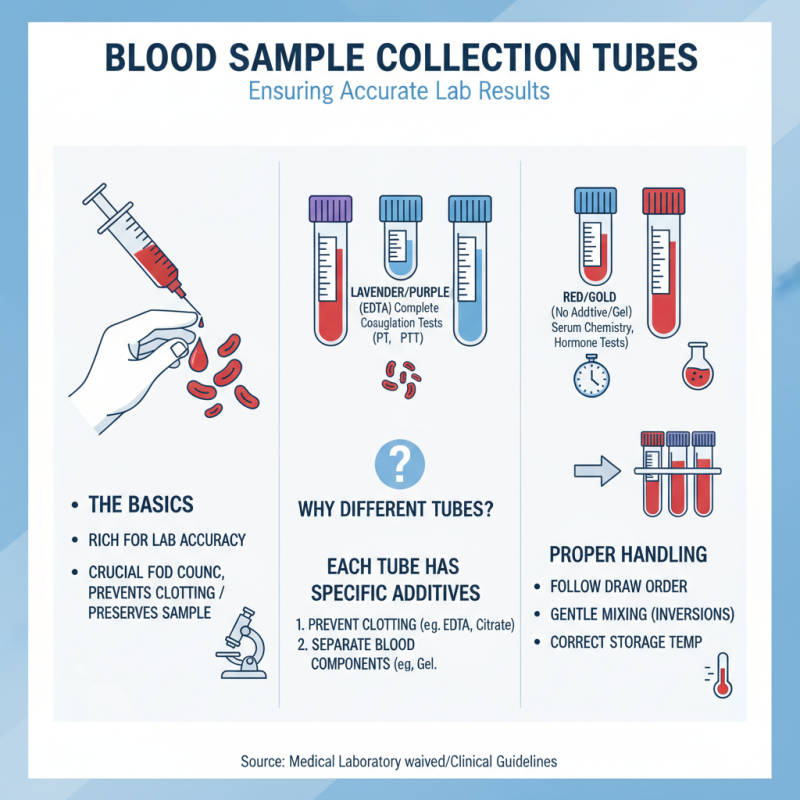
Blood sample collection tubes are crucial for accurate laboratory results. Different types exist for various tests. Understanding these tubes helps ensure proper sample collection and handling.
There are primarily two groups of tubes: those with anticoagulants and those without. Anticoagulant tubes are often colored differently. For instance, lavender tops usually contain EDTA, used for complete blood counts. Green tops often have heparin for certain chemistry tests.
It’s vital to use the correct tube for the desired test. Misuse can lead to false results. Some may think any tube works, but that’s a mistake. Venturing into the wrong tube type may yield misleading data. Collecting blood samples correctly means following guidelines closely. Even the smallest error in choosing a tube can have significant implications. Remember to inspect tubes for any cracks or leaks. Each detail matters.
Blood collection tubes play a crucial role in laboratory testing. They contain specific additives that help preserve the sample's integrity. Understanding these components is essential for accurate diagnoses.
Additives vary by tube type. For example, EDTA prevents clotting and is often used for cellular tests. Serum tubes typically contain a separator gel that aids in separating serum from cells. Each additive serves a unique purpose and can influence test results significantly.
While selecting tubes, one must pay attention to their expiration dates and storage conditions. Often overlooked, these factors can affect the sample's quality. Not evaluating these details leads to potential errors in test interpretations. Awareness of these components can improve sample collection practices.
When collecting blood samples, proper techniques ensure reliable results.
Consistency is key. Start by preparing the collection site properly.
Clean the area with an antiseptic wipe. Be sure to let it dry completely.
Drying helps prevent contamination.
Next, choose the right tube. Different tests require different additives.
Staying organized with your supplies is essential.
Sometimes, mistakes happen due to mixed-up tubes. It is crucial to double-check.
Use a gentle but firm grip on the needle.
A shaky hand can lead to unsuccessful draws and frustration.
After the sample is collected, immediately label the tube.
Include patient details and the date.
Delays can cause misidentification.
Finally, remember that learning comes from experience.
Reflect on each collection.
Being mindful of these practices improves technique over time.
Each step matters in ensuring quality samples.
The color and type of blood sample collection tubes play a crucial role in ensuring sample integrity. Different additives in tubes can affect test results significantly. For instance, the use of EDTA in purple-top tubes is essential for hematological tests. A study showed that 15% of samples collected in incorrect tubes led to inaccurate CBC results. This discrepancy can cause misdiagnosis.
Additionally, gel separator tubes, often yellow or orange, are vital for serum separation. However, if these tubes are not mixed correctly, it can lead to erroneous biochemical results. An analysis revealed that improperly mixed samples may yield a false elevation of enzymes, impacting clinical decisions. Test environments also matter; temperature fluctuations can affect additive stability.
There's a growing recognition of these issues among healthcare professionals. Many stress the need for education on correct tube usage. A survey indicated that nearly 30% of respondents believed they lacked adequate training in this area. This gap in knowledge can lead to mistakes in sample collection and processing. The potential for human error highlights the necessity for best practices in blood sample collection.
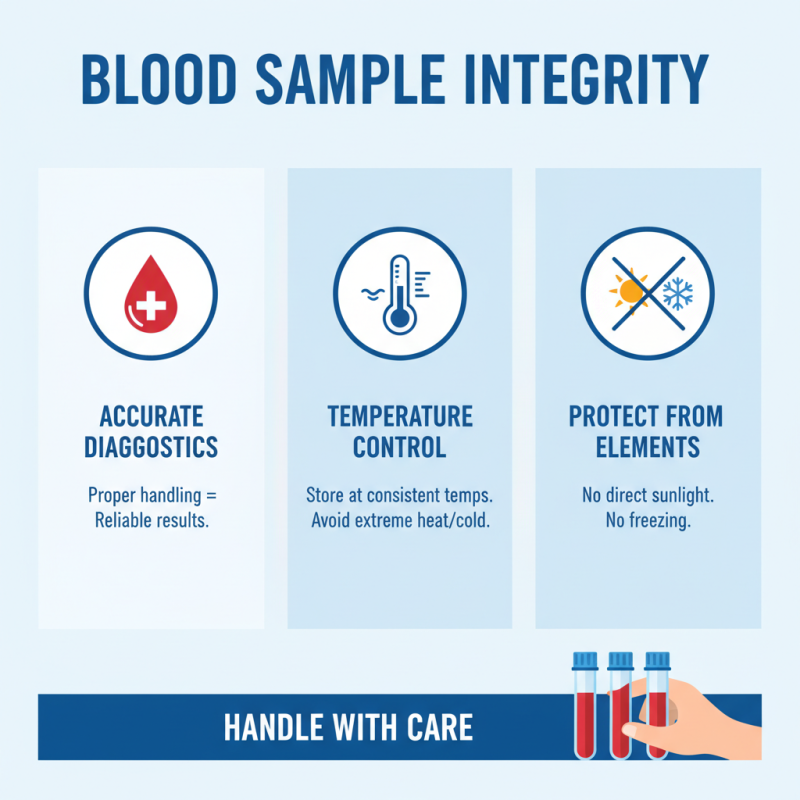
Blood samples are crucial for accurate diagnostics. Proper storage and transportation can significantly affect the results. It’s essential to handle blood collection tubes with care. Temperature fluctuations can alter sample integrity. Store tubes at consistent temperatures. Avoid exposure to direct sunlight or extreme cold.
Tips for packing samples include using insulated containers. Ensure tubes are upright during transport. This prevents mixing of sample contents. Label each tube clearly. A missing label can lead to confusion. Be aware of the shelf life of each type of tube. Using expired tubes can lead to unreliable results.
Monitor transportation time. Delay can also compromise sample quality. Make plans for prompt delivery to the lab. In emergency cases, consider alternative transport methods. Always double-check the sealing of tubes. A small leak can ruin an entire sample. Mistakes in handling can lead to extra work and wasted resources.